Varicose veins are swollen and twisted veins that often occur in the legs, resulting from weakened valves that lead to poor blood flow. For many individuals, varicose veins can cause discomfort and even lead to complications if left untreated. When conservative treatments such as lifestyle changes, compression stockings, or sclerotherapy are ineffective, surgical options may be considered. This article explores the different types of varicose vein surgery available, detailing their procedures, indications, and potential benefits.
1. Vein Stripping
A. Overview
Vein stripping is a traditional surgical method used to remove varicose veins. This procedure involves removing the affected vein through small incisions.
B. Procedure
- Anesthesia: The procedure is typically performed under general anesthesia or spinal anesthesia.
- Incisions: The surgeon makes small incisions near the groin and ankle to access the varicose vein.
- Vein Removal: The affected vein is then stripped out from the body using a specialized instrument.
- Closure: The incisions are closed with stitches or adhesive strips.
C. Indications
- Suitable for individuals with large varicose veins that cause significant discomfort or complications.
- Often recommended for those who have not responded to conservative treatments.
D. Benefits
- Effective in removing the source of varicose veins.
- Can lead to significant improvement in symptoms and appearance.
E. Risks
- As with any surgical procedure, risks include infection, bleeding, and bruising. There may also be discomfort during recovery.
2. Endovenous Laser Treatment (EVLT)
A. Overview
EVLT is a minimally invasive procedure that uses laser energy to close off varicose veins. This method is becoming increasingly popular due to its effectiveness and shorter recovery time.
B. Procedure
- Anesthesia: Local anesthesia is typically used to numb the treatment area.
- Catheter Insertion: A thin catheter is inserted into the affected vein through a small incision.
- Laser Activation: Laser energy is delivered through the catheter, causing the vein to heat up and collapse.
- Closure: The vein is sealed, and blood is rerouted to healthier veins.
C. Indications
- Suitable for individuals with large varicose veins that need treatment.
- Often recommended for those who want to avoid more invasive surgical options.
D. Benefits
- Minimally invasive with a shorter recovery time compared to traditional surgery.
- Less postoperative pain and fewer complications.
E. Risks
- Potential risks include bruising, redness, or swelling at the treatment site. There is also a small risk of blood clots.
3. Radiofrequency Ablation (RFA)
A. Overview
RFA is another minimally invasive procedure similar to EVLT, but it uses radiofrequency energy instead of lasers to close off varicose veins.
B. Procedure
- Anesthesia: Local anesthesia is applied to the treatment area.
- Catheter Insertion: A catheter is inserted into the affected vein.
- Radiofrequency Energy: Radiofrequency energy is applied through the catheter, causing the vein walls to heat up and collapse.
- Closure: The vein is sealed, allowing blood to flow through healthier veins.
C. Indications
- Suitable for larger varicose veins that require treatment.
- Often chosen by patients who prefer minimally invasive options.
D. Benefits
- Quick recovery time and minimal discomfort.
- Effective in treating symptomatic varicose veins.
E. Risks
- Similar to EVLT, risks include bruising, swelling, and potential blood clots.
4. Sclerotherapy
A. Overview
While not a surgical procedure in the traditional sense, sclerotherapy is often used to treat smaller varicose veins and spider veins. It involves injecting a solution into the affected veins to cause them to collapse.
B. Procedure
- Preparation: The area is cleaned, and a local anesthetic may be applied.
- Injection: A sclerosing agent (solution) is injected directly into the affected vein.
- Closure: The solution irritates the vein lining, causing it to seal shut and fade over time.
C. Indications
- Best suited for smaller varicose veins and spider veins.
- Often recommended for patients seeking a non-surgical treatment option.
D. Benefits
- Minimally invasive with no need for incisions.
- Quick recovery time with minimal discomfort.
E. Risks
- Risks may include temporary bruising, swelling, or skin irritation. In rare cases, complications such as allergic reactions or blood clots may occur.
5. Ambulatory Phlebectomy
A. Overview
Ambulatory phlebectomy is a minimally invasive surgical procedure used to remove superficial varicose veins through tiny incisions.
B. Procedure
- Anesthesia: Local anesthesia is typically used.
- Incisions: Small incisions are made along the affected vein.
- Vein Removal: The varicose vein is carefully removed using specialized hooks or tools.
- Closure: The incisions are closed, often without the need for stitches.
C. Indications
- Suitable for patients with smaller, superficial varicose veins.
- Often used in conjunction with other treatments, such as sclerotherapy or EVLT.
D. Benefits
- Minimally invasive with a quick recovery time.
- Effective for removing surface varicose veins without significant scarring.
E. Risks
- Risks include infection, bruising, or temporary discomfort at the incision sites.
Understanding the different types of varicose vein surgery can empower individuals to make informed decisions about their treatment options. The choice of procedure will depend on various factors, including the size and severity of the varicose veins, individual health conditions, and personal preferences. Consulting with a healthcare provider or vascular specialist is essential to determine the most appropriate course of action for effective treatment and management of varicose veins.
Frequently Asked Questions (FAQ)
1. What are the signs that I may need surgery for varicose veins?
Signs may include chronic pain, swelling, skin changes, and complications like blood clots or ulcers that do not improve with conservative treatments.
2. How do I know which surgery is right for me?
Consult with a vascular specialist who can evaluate your specific condition, discuss treatment options, and recommend the best approach based on your needs.
3. What is the recovery time for varicose vein surgery?
Recovery time varies by procedure but generally ranges from a few days to a couple of weeks. Minimally invasive procedures like EVLT and RFA typically have shorter recovery times compared to vein stripping.
4. Are there risks associated with varicose vein surgery?
Yes, as with any surgical procedure, there are risks, including infection, bleeding, bruising, and, in rare cases, complications like blood clots.
5. Can varicose veins come back after surgery?
While surgery can significantly reduce or eliminate existing varicose veins, new ones may develop over time due to genetic or lifestyle factors.
6. Is sclerotherapy effective for treating larger varicose veins?
Sclerotherapy is generally more effective for smaller varicose veins and spider veins. Larger varicose veins may require surgical intervention or other treatments like EVLT or RFA.
7. How should I prepare for varicose vein surgery?
Your healthcare provider will give you specific instructions, which may include avoiding certain medications, arranging for transportation home after the procedure, and following pre-operative guidelines.
8. Can I resume normal activities after varicose vein surgery?
Most patients can return to light activities shortly after minimally invasive procedures. However, strenuous exercise and heavy lifting may need to be avoided for a period as recommended by your healthcare provider.
9. Will insurance cover varicose vein surgery?
Coverage varies by insurance provider and plan. It's important to check with your insurance company to understand your benefits and any out-of-pocket costs.
10. What lifestyle changes can help prevent varicose veins from developing?
Maintaining a healthy weight, exercising regularly, wearing compression stockings, and avoiding prolonged sitting or standing can help reduce the risk of developing varicose veins.
 Clinic Booking
Clinic Booking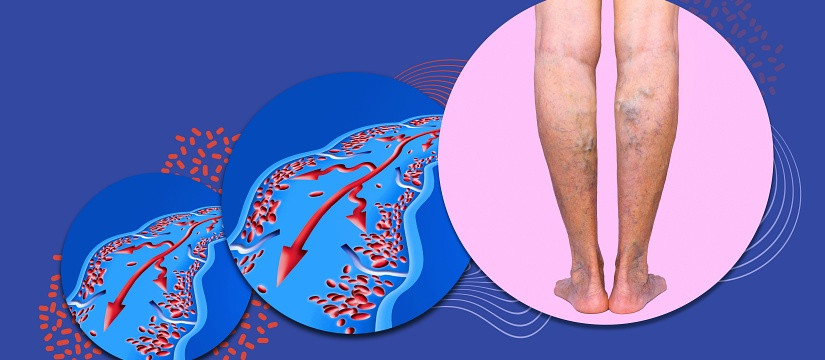


 No Record
No Record