Pacemakers are vital medical devices designed to regulate heart rhythms, especially for individuals with conditions like bradycardia (slow heart rate) and heart block. Although modern pacemakers are generally reliable, there can be instances when they do not function correctly. Recognizing the signs that your pacemaker may not be working as intended is crucial for timely intervention and maintaining your heart health. This article explores the common signs and symptoms to watch for, along with guidance on when to seek medical attention.
1. Understanding Your Pacemaker
1.1 What is a Pacemaker?
A pacemaker is a small electronic device implanted under the skin of the chest. It helps control the heart's electrical activity by sending electrical impulses to ensure the heart maintains a normal rhythm. Pacemakers are commonly used to treat conditions such as:
- Bradycardia: A condition where the heart beats too slowly.
- Heart Block: A delay or blockage in the heart's electrical signals.
- Atrial Fibrillation: An irregular heart rhythm that can lead to other complications.
1.2 Importance of Monitoring
Regular monitoring and follow-up appointments are essential for ensuring that your pacemaker functions correctly. Awareness of potential malfunction signs can help you take prompt action and avoid complications that could affect your health.
2. Common Signs Your Pacemaker May Not Be Functioning Properly
2.1 Unusual Heart Rhythms
- Palpitations: An increased awareness of your heart beating, often described as fluttering, pounding, or racing. Frequent or prolonged palpitations may indicate that the pacemaker is not maintaining a stable rhythm.
- Dizziness or Fainting: Experiencing lightheadedness, dizziness, or fainting spells could suggest that the pacemaker is not providing adequate pacing. This is particularly concerning if it occurs suddenly or frequently.
2.2 Changes in Heart Rate
- Sudden Changes: If you notice a sudden increase or decrease in your heart rate, this could indicate that the pacemaker is malfunctioning. A heart rate consistently lower than what is set on the device may signify inadequate pacing.
- Bradycardia Symptoms: Symptoms such as fatigue, weakness, or confusion may arise if your heart rate drops below the pacemaker's programmed rate. It’s essential to be vigilant about these signs.
2.3 Persistent Pain or Discomfort
- Incision Site Pain: Ongoing or worsening pain at the incision site may indicate complications, such as infection or device displacement. Monitoring the area for unusual changes is crucial.
- Chest Discomfort: New or unusual chest pain that differs from your usual symptoms should not be ignored, as it may signal that the pacemaker is not functioning correctly or that there is another underlying issue.
2.4 Device-Related Issues
- Lead Displacement: If the leads that connect the pacemaker to the heart become dislodged, it can impair the device's ability to sense and pace the heart correctly. Symptoms of lead displacement may include palpitations, dizziness, or fainting.
- Battery Depletion: Pacemakers typically have a lifespan of 5 to 15 years. If the battery is running low, you may experience symptoms similar to those of bradycardia, along with warnings from the device during check-ups.
2.5 Signs of Infection
- Redness and Swelling: Increased redness, swelling, or warmth around the incision site may indicate an infection, which can impact the device's function. Watch for these signs, especially in the days and weeks following the procedure.
- Fever: A fever or systemic symptoms (such as chills) accompanying localized symptoms may suggest an infection related to the pacemaker.
3. When to Seek Medical Attention
3.1 Immediate Consultation
If you experience any of the following symptoms, it’s crucial to seek medical attention promptly:
- Persistent dizziness or fainting spells
- Unusual or severe chest pain
- Continuous palpitations or irregular heartbeats
- Signs of infection at the incision site (redness, swelling, fever)
- Sudden changes in heart rate that last more than a few minutes
3.2 Regular Follow-Ups
Regular follow-up appointments are essential to monitor your pacemaker’s function. Your healthcare provider may recommend checks every 6 to 12 months, or more frequently if you experience any concerning symptoms.
4. Understanding Device Monitoring
4.1 Regular Check-Ups
During follow-up appointments, healthcare providers conduct several evaluations to assess the pacemaker's functionality:
- Device Interrogation: This process involves using a specialized programmer to communicate with the pacemaker. The provider retrieves data about the device's performance, including battery life, lead function, and any recorded arrhythmias or pacing events.
- Lead Testing: The leads that connect the pacemaker to the heart are tested to ensure they are correctly positioned and functioning properly. This may include checking for lead impedance and sensing capabilities.
4.2 Assessing Heart Health
- Electrocardiogram (ECG): An ECG may be performed during follow-up appointments to monitor the heart's electrical activity. This test helps confirm that the pacemaker is effectively managing the heart rate.
- Review of Symptoms: Healthcare providers will ask about any symptoms you may have experienced, such as dizziness, palpitations, or fatigue, which can help assess the effectiveness of the pacemaker.
5. Long-Term Considerations
5.1 Regular Monitoring
Long-term success with a pacemaker relies on ongoing monitoring and lifestyle management. Patients should be proactive in keeping track of their symptoms and maintaining open communication with their healthcare team.
5.2 Lifestyle Adjustments
In addition to regular monitoring, making certain lifestyle adjustments can help optimize the function of your pacemaker:
- Adhering to Medication: Always take prescribed medications as directed, as they can help manage your heart condition and support the pacemaker’s effectiveness.
- Healthy Living: Focus on a heart-healthy lifestyle, including regular exercise, a balanced diet, and stress management techniques to improve overall cardiovascular health.
Recognizing the signs that your pacemaker may not be functioning properly is vital for maintaining heart health and preventing complications. Being aware of symptoms such as unusual heart rhythms, changes in heart rate, persistent pain or discomfort, and signs of infection can empower you to seek timely medical attention. Regular follow-up appointments are essential for monitoring the device's performance and ensuring optimal heart function. Always communicate with your healthcare provider regarding any concerns or symptoms you may experience after receiving your pacemaker.
Frequently Asked Questions (FAQ)
1. What are the signs that my pacemaker is not working properly?
Signs include unusual heart rhythms, dizziness, fainting, persistent pain at the incision site, changes in heart rate, and signs of infection.
2. How can I tell if my heart rate is too low?
If you feel excessively tired, weak, or dizzy, or if you notice a consistent heart rate lower than your pacemaker's set rate, it may indicate an issue.
3. What should I do if I experience palpitations or irregular heartbeats?
Contact your healthcare provider immediately if you experience palpitations or any irregular heartbeats that are new or concerning.
4. How often should I have my pacemaker checked?
Regular follow-up appointments are typically scheduled every 6 to 12 months, but you should consult your healthcare provider for specific recommendations based on your condition.
5. Are there any specific activities I should avoid if I suspect my pacemaker isn’t working?
If you suspect a malfunction, it’s best to avoid strenuous activities until assessed by a healthcare provider.
6. Can a pacemaker get infected?
Yes, infections can occur at the incision site or internally with the device. Monitoring for signs of infection is essential after implantation.
7. How long does a pacemaker last?
Pacemakers usually last between 5 to 15 years, depending on usage and the specific type of device.
8. Is it safe to engage in sexual activity after getting a pacemaker?
Most patients can resume sexual activity shortly after recovery, but it’s important to consult with your healthcare provider regarding any specific concerns.
9. Can I travel with a pacemaker?
Yes, traveling is generally safe for patients with pacemakers, but it’s advisable to consult your healthcare provider before traveling and carry your pacemaker identification card.
10. What should I do if I notice changes in my symptoms after getting a pacemaker?
Contact your healthcare provider immediately if you notice any new or worsening symptoms, such as chest pain, significant changes in heart rhythm, or severe dizziness.
 Clinic Booking
Clinic Booking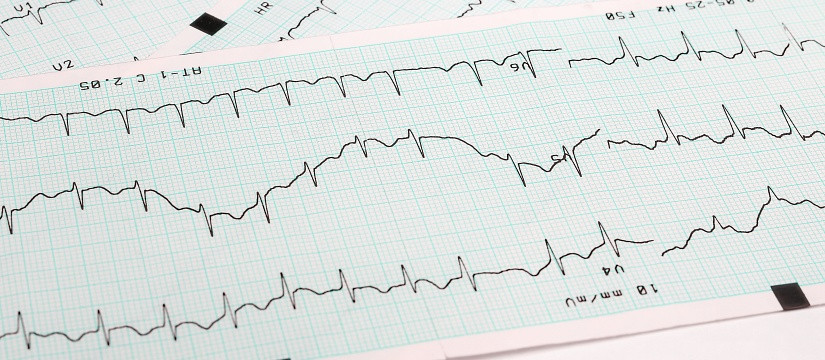


 No Record
No Record