Hip replacement surgery, or hip arthroplasty, is a prevalent and effective procedure performed to alleviate pain and restore mobility in individuals suffering from severe hip joint damage. A common concern among patients considering this surgery is the duration of the procedure. Understanding how long the surgery takes, along with the factors that can influence this timeline, can help patients prepare for their surgical experience and recovery.
Overview of Hip Replacement Surgery Duration
Average Surgery Time
The typical duration of hip replacement surgery generally ranges from 1 to 2 hours. This timeframe refers specifically to the surgical procedure itself and does not include preoperative preparations or postoperative recovery time.
Factors Influencing Surgery Duration
Several factors can affect the length of hip replacement surgery, including:
Type of Hip Replacement:
- Total Hip Replacement (THR): Involves replacing both the femoral head and the acetabulum, typically taking longer due to the complexity of the procedure.
- Partial Hip Replacement (Hemiarthroplasty): Generally shorter, as only the femoral head is replaced.
- Hip Resurfacing: Can take a similar duration to total hip replacement but may vary based on the surgical technique employed.
Surgical Approach:
- Traditional Approach: The posterior or lateral approach may require more time due to the need for more extensive muscle and tissue manipulation.
- Minimally Invasive Approach: The anterior approach can potentially reduce surgery time and improve recovery due to less disruption of surrounding tissues.
Surgeon’s Experience:
- The proficiency and experience of the surgeon can influence the speed and efficiency of the procedure. More experienced surgeons may perform the surgery more quickly due to their familiarity with techniques and anatomy.
Patient Factors:
- Individual patient anatomy, such as the condition of the hip joint, bone density, and previous surgeries, can affect how long the surgery takes. Complex cases may require additional time to address specific issues.
Use of Technology:
- Advanced surgical techniques, including computer-assisted surgery or robotic assistance, can improve precision but may also affect the overall duration.
Timeline for the Surgical Process
Understanding the entire surgical process can provide patients with a clearer picture of what to expect on the day of the procedure.
1. Preoperative Preparations (1-2 Hours)
- Preoperative Assessment: Before surgery, patients will undergo a thorough assessment, which may include a review of medical history, physical examination, and imaging studies (X-rays or MRIs) to evaluate the condition of the hip joint and guide the surgical plan.
- Medical Optimization: If necessary, patients may be advised to lose weight, manage chronic conditions (such as diabetes or hypertension), and quit smoking to improve surgical outcomes.
- Anesthesia Consultation: Patients will meet with an anesthesiologist to discuss the type of anesthesia that will be used during surgery, which may include general or regional anesthesia.
- Final Preparations: Patients will change into a hospital gown, and intravenous (IV) lines will be placed for medication administration.
2. Surgical Procedure (1-2 Hours)
Anesthesia Administration: Once the patient is in the operating room, the chosen anesthesia is administered to ensure comfort and pain relief throughout the procedure.
Incision: The surgeon makes an incision over the hip joint, typically about 6 to 10 inches long, depending on the surgical approach used. This incision allows access to the hip joint while minimizing damage to surrounding muscles and tissues.
Accessing the Hip Joint: The surgeon carefully moves aside the muscles and soft tissues surrounding the hip joint to gain access to the joint. In some approaches, such as the anterior method, muscles are preserved rather than cut.
Removal of Damaged Tissue: The damaged femoral head and acetabulum are removed, and any debris or loose cartilage is cleaned out to prepare the area for the new implants.
Implant Placement: The surgeon inserts the artificial components:
- Femoral Component: A metal stem is placed into the femur (thigh bone) with a new femoral head attached.
- Acetabular Component: A cup-shaped implant is inserted into the acetabulum (hip socket).
Closure: After verifying the proper alignment and stability of the implants, the surgeon closes the incision using stitches or staples, and a sterile dressing is applied.
3. Postoperative Recovery (2-4 Hours)
- Recovery Room: After surgery, patients are moved to a recovery area where they are monitored as they wake from anesthesia. Vital signs, pain levels, and overall condition will be assessed regularly.
- Initial Mobility: Once patients are stable and awake, they may begin gentle movements and physical therapy, usually within the same day. The healthcare team will encourage patients to start moving their legs and begin sitting up as soon as possible to promote circulation.
3. Early Recovery Phase (Weeks 1-2)
Home Care
- Discharge Planning: Before leaving the hospital, a discharge plan will be developed, including instructions for home care, medication management, and follow-up appointments.
- Home Modifications: It may be helpful to make home modifications, such as removing tripping hazards and arranging furniture for easier mobility.
Pain and Swelling Management
- Ongoing Pain: Some pain and swelling are common in the initial weeks. Ice therapy can help reduce swelling, and pain medications should be taken as prescribed.
- Activity Limitations: Patients should avoid high-impact activities and heavy lifting during this phase to promote healing.
Physical Therapy and Rehabilitation
- Exercises: Physical therapy will continue, focusing on strength, range of motion, and functional activities. Patients may start with seated exercises and progress to standing and walking.
- Goals: The goal is to regain independence in daily activities and improve mobility.
4. Intermediate Recovery Phase (Weeks 3-6)
Increasing Activity Levels
- Walking and Mobility: Patients can expect to walk more independently and increase their activity levels during this phase. Most individuals can gradually transition from assistive devices to walking without assistance.
- Functional Activities: Patients can begin engaging in more daily activities, such as climbing stairs and getting in and out of vehicles.
Continued Physical Therapy
- Strength Building: Physical therapy will focus on building strength in the hip and surrounding muscles, as well as improving balance and coordination.
- Home Exercises: Patients may be given a home exercise program to continue their rehabilitation progress outside of formal therapy sessions.
Monitoring Progress
- Follow-Up Appointments: Regular follow-up appointments with the orthopedic surgeon will be scheduled to monitor healing, assess range of motion, and address any concerns.
5. Long-Term Recovery Phase (3-6 Months)
Continued Improvement
- Range of Motion: Most patients experience significant improvements in range of motion and functionality during this phase.
- Pain Reduction: By this time, many individuals report a substantial reduction in pain, often achieving a level of pain relief that allows them to engage in previously enjoyed activities.
Resuming Daily Activities
- Return to Normal Activities: Patients can expect to return to many daily activities, including walking, swimming, and other low-impact exercises. However, high-impact sports should be avoided to protect the implant.
- Gradual Resumption of Hobbies: Depending on individual progress, many patients can gradually resume hobbies and recreational activities.
6. Potential Challenges
Common Postoperative Concerns
- Swelling and Stiffness: Some swelling and stiffness may persist, particularly after prolonged periods of inactivity or excessive activity.
- Emotional Adjustments: Emotional challenges, such as frustration or anxiety about mobility, are common. It’s important for patients to communicate these feelings with their healthcare team.
Monitoring for Complications
- Signs of Infection: Patients should watch for signs of infection, such as increased redness, warmth, swelling, or discharge from the incision site, as well as fever.
- Blood Clots: Awareness of potential signs of blood clots (e.g., swelling, pain, or warmth in the calf) is crucial, and patients should follow their physician’s instructions regarding blood thinner medications.
7. Tips for a Successful Recovery
1. Follow Your Rehabilitation Plan
- Adhere to the prescribed physical therapy and exercise regimen to ensure optimal recovery.
2. Prioritize Nutrition
- Eat a balanced diet rich in nutrients to support healing and overall health. Focus on foods that provide calcium and vitamin D for bone health.
3. Stay Hydrated
- Drink plenty of water to stay hydrated and support your body during the recovery process.
4. Manage Pain Effectively
- Take pain medications as prescribed and communicate any concerns about pain management with your healthcare provider.
5. Listen to Your Body
- Pay attention to your body’s signals. Rest when needed and avoid overexertion to prevent setbacks in recovery.
6. Maintain Open Communication
- Keep an open line of communication with your healthcare team. Discuss any issues, fears, or uncertainties with your healthcare team to ensure a comprehensive approach to your recovery.
Understanding the typical duration and process of hip replacement surgery can help patients prepare for their recovery journey. With a clear expectation of what to expect before, during, and after the procedure, individuals can approach their surgery with greater confidence. By actively participating in rehabilitation and following medical advice, patients can achieve successful outcomes and enjoy an improved quality of life post-surgery.
Frequently Asked Questions (FAQ)
1. How long does hip replacement surgery typically take?
The surgery usually lasts between 1 to 2 hours, depending on various factors.
2. What factors can influence the duration of the surgery?
Factors include the type of hip replacement, surgical approach, surgeon’s experience, patient anatomy, and the use of technology.
3. What is the average time spent in the hospital after hip replacement surgery?
Most patients stay in the hospital for 1 to 3 days after surgery for monitoring and recovery.
4. Does the surgical approach affect the duration of the surgery?
Yes, the surgical approach can influence the time taken for the procedure. Minimally invasive techniques may reduce surgery time.
5. What happens in the recovery room after surgery?
Patients are monitored in the recovery room as they wake from anesthesia, with vital signs checked and pain management implemented.
6. When will I start physical therapy after surgery?
Physical therapy usually begins within 24 to 48 hours after surgery to promote early mobilization.
7. Will I feel pain during the surgery?
Anesthesia will be administered to ensure that you do not feel pain during the surgery.
8. Can I expect a quick recovery after surgery?
While many patients experience a significant improvement in mobility and pain relief, full recovery typically takes 3 to 6 months.
9. How can I prepare for my surgery to ensure it goes smoothly?
Prepare by following your surgeon's preoperative instructions, discussing any concerns, and ensuring you have a support system in place for recovery.
10. What can I do if I have further questions about the procedure?
It’s essential to communicate openly with your healthcare team to address any questions or concerns before the surgery.
 Clinic Booking
Clinic Booking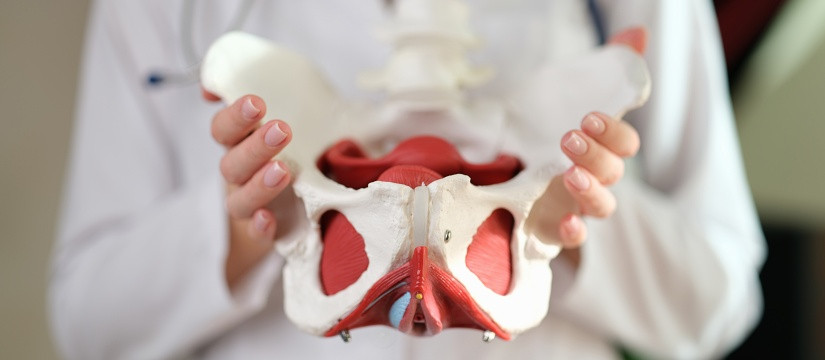


 No Record
No Record