Endovascular Aneurysm Repair (EVAR) is a minimally invasive surgical procedure used to treat abdominal aortic aneurysms (AAA) and, in some cases, thoracic aortic aneurysms (TAA). This technique involves the placement of a stent-graft within the affected artery through small incisions, typically in the groin or arm, to reinforce the weakened section of the blood vessel and prevent rupture. Understanding the EVAR procedure, its indications, benefits, risks, and recovery process is essential for patients considering this treatment option.
1. Understanding Abdominal Aortic Aneurysms (AAA)
A. Definition
An abdominal aortic aneurysm is a dilation or bulging in the wall of the aorta as it passes through the abdomen. AAAs can be life-threatening if they rupture, leading to severe internal bleeding. Many patients with AAAs may remain asymptomatic until the aneurysm grows large or ruptures.
B. Risk Factors
Common risk factors for developing an AAA include:
- Age (typically over 65 years)
- Male gender
- Family history of aneurysms
- Smoking
- High blood pressure
- High cholesterol
- Atherosclerosis (hardening of the arteries)
2. Indications for EVAR
A. When is EVAR Recommended?
EVAR is typically indicated for patients with:
- Aortic aneurysms that measure 5.5 cm or larger.
- Smaller aneurysms that are growing rapidly (more than 0.5 cm in six months).
- Aneurysms that are symptomatic, causing pain or other complications.
- Patients who are at higher risk for complications from open surgical repair due to age or other health issues.
3. The EVAR Procedure
A. Preoperative Preparation
Before the EVAR procedure, patients undergo a thorough evaluation, which includes:
- Medical History and Physical Examination: Assessing overall health and identifying risk factors.
- Imaging Studies: CT scans or ultrasounds are performed to determine the size and shape of the aneurysm and to plan the procedure.
- Preoperative Testing: Blood tests and other assessments may be required to ensure the patient is fit for surgery.
B. The Procedure Steps
-
Anesthesia: Patients are usually given general anesthesia or sedation, depending on their health and the complexity of the procedure.
-
Incision: Small incisions (typically 1-2 inches) are made in the groin to access the femoral arteries. In some cases, an incision may be made in the arm.
-
Accessing the Aorta: A catheter is inserted into the femoral artery and guided through the blood vessels to the site of the aneurysm using fluoroscopic imaging for guidance.
-
Stent-Graft Placement: The stent-graft, a fabric tube supported by a metal mesh framework, is delivered through the catheter to the aneurysm site. Once in position, the stent-graft is expanded to fit snugly against the artery wall, sealing off the aneurysm from the bloodstream.
-
Confirming Placement: Imaging tests are used to ensure the stent-graft is positioned correctly and there are no leaks.
-
Closing the Incisions: The incisions are closed with sutures or adhesive strips, and the patient is moved to recovery for monitoring.
4. Benefits of EVAR
- Minimally Invasive: Compared to traditional open surgery, EVAR involves smaller incisions, leading to less pain, reduced scarring, and shorter recovery times.
- Shorter Hospital Stay: Most patients can go home within 1 to 2 days after the procedure, compared to a longer hospital stay required for open surgical repair.
- Quicker Recovery: Patients typically resume normal activities more quickly than those who undergo open surgery.
5. Risks and Complications
While EVAR is generally safe, there are potential risks and complications, including:
- Endoleak: A condition where blood continues to flow into the aneurysm sac, which may require additional intervention.
- Graft Migration: The stent-graft may move from its original position, potentially requiring further surgery.
- Infection: As with any surgical procedure, there is a risk of infection at the incision site.
- Thrombosis: The formation of blood clots can occur, potentially leading to complications.
- Renal Impairment: In rare cases, kidney function may be affected, particularly in patients with pre-existing conditions.
6. Postoperative Care and Recovery
A. Monitoring
- Patients will be closely monitored in the recovery area for vital signs and any complications. Follow-up imaging (such as ultrasound or CT scans) is usually performed within a few months post-surgery to check the stent-graft’s position and ensure there are no leaks.
B. Activity Restrictions
- Patients are typically advised to avoid strenuous activities, heavy lifting, and vigorous exercise for several weeks following the procedure. Gradual resumption of normal activities is encouraged based on the surgeon's recommendations.
C. Medications
- Pain management and medications to prevent blood clots (anticoagulants) may be prescribed to support recovery.
Endovascular Aneurysm Repair (EVAR) is a valuable and effective treatment option for managing abdominal aortic aneurysms, especially in patients who are at higher risk for open surgery. Understanding the procedure, its indications, benefits, and potential risks can empower patients to make informed decisions about their healthcare. If you have been diagnosed with an aneurysm or are at risk, it is essential to consult with a healthcare professional to discuss the most appropriate treatment options for your situation.
Frequently Asked Questions (FAQ)
1. What is EVAR?
Endovascular Aneurysm Repair (EVAR) is a minimally invasive surgical procedure used to treat abdominal aortic aneurysms (AAA) by placing a stent-graft inside the affected artery.
2. When is EVAR recommended?
EVAR is recommended for larger aneurysms (typically ≥ 5.5 cm), rapidly growing aneurysms, or symptomatic aneurysms, particularly in patients at higher risk for complications from open surgery.
3. How is the EVAR procedure performed?
The procedure involves making small incisions in the groin to access the femoral arteries, guiding a stent-graft to the aneurysm site using a catheter, and deploying the stent-graft to reinforce the artery wall.
4. What are the benefits of EVAR compared to open surgery?
EVAR is minimally invasive, resulting in shorter recovery times, reduced pain, less scarring, and a shorter hospital stay compared to traditional open surgical repair.
5. What are the risks associated with EVAR?
Potential risks include endoleak, graft migration, infection, thrombosis, and, in rare cases, renal impairment.
6. How long is the recovery time after EVAR?
Most patients can return home within 1 to 2 days after the procedure and typically resume normal activities within a few weeks, depending on individual recovery.
7. Will I need follow-up care after EVAR?
Yes, follow-up imaging studies are usually performed within a few months post-surgery to monitor the stent-graft's position and assess for complications.
8. Can I have an EVAR if I have other medical conditions?
Each case is assessed individually. Patients with other medical conditions may still be candidates for EVAR, but this will be determined by the healthcare team.
9. What should I do if I experience symptoms after EVAR?
If you notice any unusual symptoms, such as severe pain, swelling, or changes in color in the legs, contact your healthcare provider immediately.
10. How can I reduce my risk of developing an abdominal aortic aneurysm?
Maintaining a healthy lifestyle, managing blood pressure, avoiding smoking, and undergoing regular medical check-ups can help reduce the risk of developing an AAA.
 Clinic Booking
Clinic Booking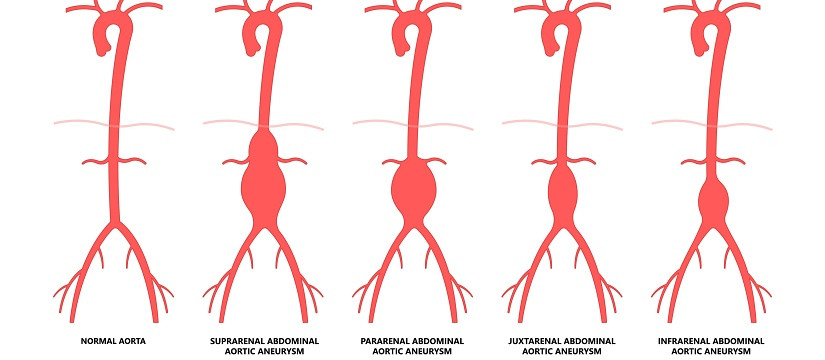


 No Record
No Record